What is it?
Coronaviruses are a type of virus found in animals and people. At the end of 2019, a novel coronavirus was identified as the cause of a cluster of pneumonia cases in Wuhan, a city in the Hubei Province of China. It rapidly spread, resulting in an epidemic throughout China, followed by an increasing number of cases in other countries throughout the world. In February 2020, the World Health Organization designated the disease COVID-19, which stands for coronavirus disease 2019
How is it spread?
Person-to-person spread is thought to occur mainly via respiratory droplets.
With droplet transmission, virus released in the respiratory secretions when a person with infection coughs, sneezes, or talks can infect another person if it makes direct contact with the mucous membranes; infection can also occur if a person touches an infected surface and then touches his or her eyes, nose, or mouth.
Droplets typically do not travel more than six feet (about two meters) and do not linger in the air
What are the symptoms?
The incubation period for COVID-19 is thought to be within 14 days following exposure, with most cases occurring approximately four to five days after exposure
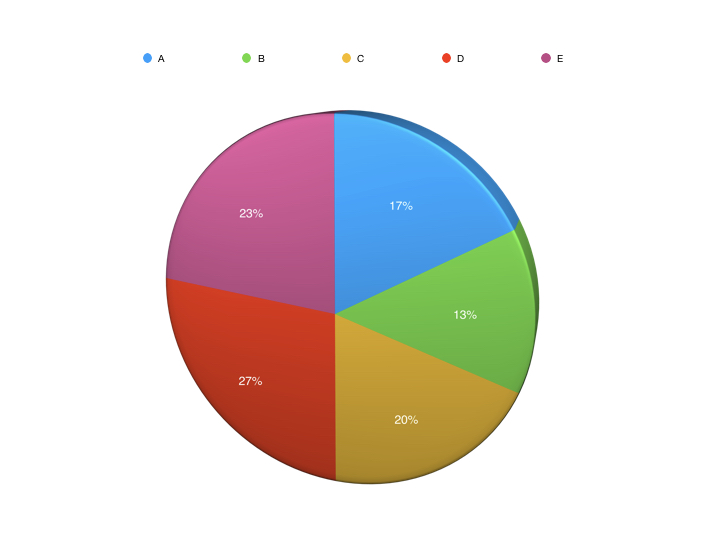
Fever in 99%
Fatigue in 70%
Dry cough in 59%
Loss of appetite in 40%
Myalgias (muscular pains) in 35%
Dyspnea (shortness of breath) in 31%
Sputum production in 27%
How serious is it?
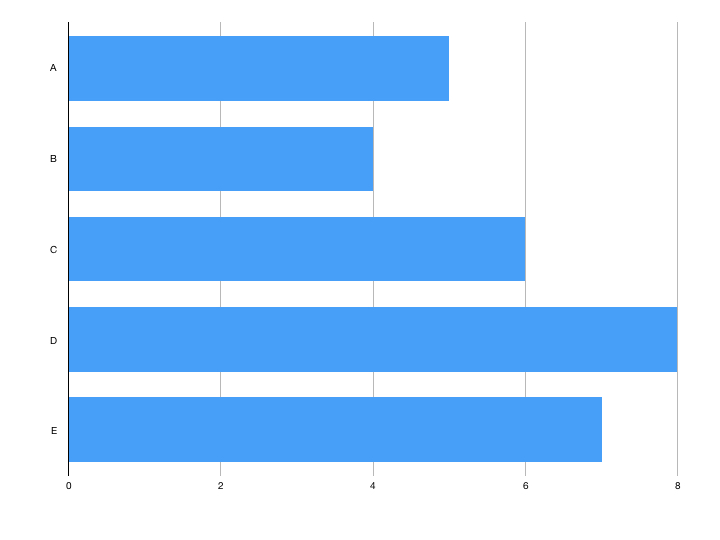
Mild (no or mild pneumonia) 81%
Severe disease (eg, with dyspnea, hypoxia, or >50 percent lung involvement on imaging within 24 to 48 hours) 14%
Critical disease (eg, with respiratory failure, shock, or multi-organ dysfunction) 5%
Overall case fatality rate 2.3%
Prevention
The following general measures are recommended to reduce transmission of infection:
Diligent hand washing, particularly after touching surfaces in public
Use of hand sanitizer that contains at least 60 percent alcohol is a reasonable alternative if the hands are not visibly dirty
Respiratory hygiene (eg, covering the cough or sneeze)
Avoiding touching the face (in particular eyes, nose, and mouth)
Avoiding crowds
Cleaning and disinfecting objects and surfaces that are frequently touched
Self-isolation
If you live alone and you have symptoms of coronavirus illness (COVID-19), however mild, stay at home for 7 days from when your symptoms started
If you live with others and you are the first in the household to have symptoms of coronavirus, then you must stay at home for 7 days, but all other household members who remain well must stay at home and not leave the house for 14 days. The 14-day period starts from the day when the first person in the house became ill
For anyone else in the household who starts displaying symptoms, they need to stay at home for 7 days from when the symptoms appeared, regardless of what day they are on in the original 14 day isolation period
Personal Protective Equipment (PPE)
Any personnel entering the room of a patient with suspected or confirmed COVID-19 should wear the appropriate personal protection equipment: gown, gloves and a face mask
Respirators (FFP3) should be worn during aerosol-generating procedures
Aerosol-generating procedures include tracheal intubation, noninvasive ventilation, tracheotomy, cardiopulmonary resuscitation, manual ventilation before intubation, upper endoscopy, and bronchoscopy
Nasopharyngeal or oropharyngeal specimen collection is not considered an aerosol-generating procedure
Testing
The virus is detected by reverse-transcription polymerase chain reaction
A positive test confirms the diagnosis of COVID-19
If initial testing is negative but the suspicion for COVID-19 remains, the WHO recommends resampling and testing from multiple respiratory tract sites
The accuracy and predictive values of testing have not been systematically evaluated. Negative RT-PCR tests on oropharyngeal swabs despite CT findings suggestive of viral pneumonia have been reported in some patients who ultimately tested positive
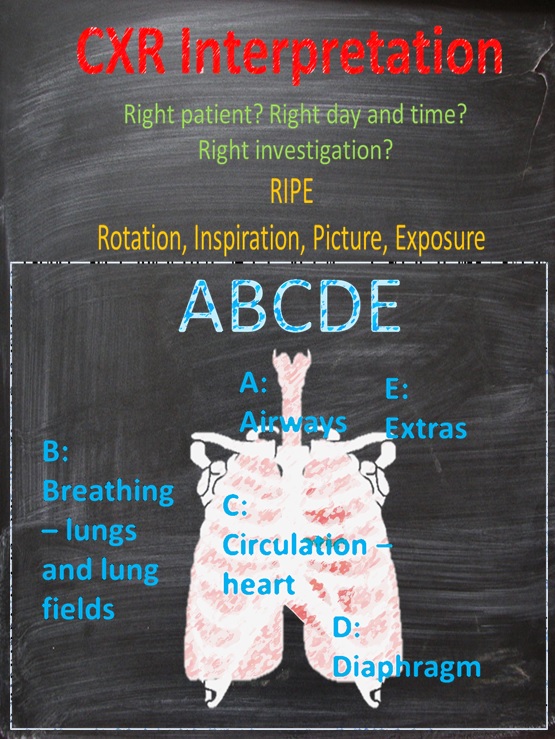
Radiological Findings
Chest CT in patients with COVID-19 most commonly demonstrates ground-glass opacification with or without consolidative abnormalities, consistent with viral pneumonia
Case series have suggested that chest CT abnormalities are more likely to be bilateral, have a peripheral distribution, and involve the lower lobes
Less common findings include pleural thickening, pleural effusion, and lymphadenopathy
In Pregnancy
In two reports including a total of 18 pregnant women with suspected or confirmed COVID-19 pneumonia, there was no laboratory evidence of transmission of the virus to the neonate
However, neonatal cases of infection have been documented
What are the risks of COVID-19 infection in pregnant women?
The approach to prevention, evaluation, diagnosis, and treatment of pregnant women with suspected COVID-19 should be similar to that in nonpregnant individuals
It is unknown whether the virus can be transmitted through breast milk. The only report of testing found no virus in the maternal milk of six patients
However, droplet transmission could occur during breastfeeding. Mothers with confirmed COVID-19 or with suspected COVID-19 should take precautions to prevent transmission to the infant during breastfeeding (including hand hygiene and use of a face mask)
Medications
Patients receiving angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) should continue treatment with these agents
Stopping these agents in some patients may exacerbate cardiovascular or kidney disease and lead to increased mortality
The decision to discontinue prednisone, biologics, or other immunosuppressive drugs in the setting of infection must be determined on a case-by-case basis. Glucocorticoids should not be used in patients with COVID-19 pneumonia unless there are other indications (eg, exacerbation of chronic obstructive pulmonary disease)
The European Medicines Agency (EMA) and the WHO do not recommend that NSAIDs be avoided when clinically indicated
How Good is the Test?
The polymerase chain reaction (PCR) test works by multiplying and then identifying viral DNA.
No test is perfect and swabs from the nose have a false negative (a negative result when the patient actually has COVID-19) rate of 37%
Throat swabs have a false negative rate of 68%
This means in patients with strong clinical suspicion of COVID-19 but a negative swab repeat testing is recommended. In patients with mild symptoms who do not require hospital admission testing with a high risk of a false negative result might be falsely reassuring
Antibody testing, currently in development, would look for antibodies to COVID-19 showing that someone has had the virus and recovered.
Is the NHS being denied personal protective equipment?
Public Health England guidance on PPE follows that of the World Health Organisation (WHO) a non-partisan specialised agency of the United Nations responsible for international public health. WHO guidance is based on all available evidence
Unfortunately, there has been a lot of media coverage stating that this guidance is not adequate. This is personal opinion being presented as fact. As with all healthcare equipment PPE is a finite resource and meeting demand will be a challenge
It is worth mentioning that even with PPE special care must be take especially during donning (putting on) and doffing (taking off). PHE have produced videos showing donning and doffing techniques
Is anosmia a symptom?
There is interest in whether anosmia (loss of sense of smell) is an important symptom of COVID-19.
There are reports of anosmia being the only symptom of infection
In Germany it is reported that more than 2 in 3 confirmed cases have anosmia. In South Korea, where testing has been more widespread, 30% of patients testing positive have had anosmia as their major presenting symptom in otherwise mild cases
However, 40% of all cases of anosmia are due to viral infections so this is not surprising. The olfactory bulb has stem cells and so regenerates in 7 to 10 days
Why is it so bad in Italy?
In Italy in mid-March the estimated fatality rate was 7.2% compared to 0.9% in South Korea at the same time. What is different about Italy?
We know that risk of mortality due to COVID-19 increases with age
Certain co-morbidities also increase mortality:
Cardiovascular disease
Diabetes mellitus
Hypertension
Chronic lung disease
Cancer
Chronic kidney disease
In Italy, the median age of patients with infection was 64 years, whereas in South Korea the median age was in the 40s. In a subset of 355 patients who died with COVID-19 in Italy, the mean number of pre-existing co-morbidities was 2.7, and only 3 patients had no underlying condition
So it seems that Italy's higher mortality rate is due to the disease's prevalence in an older population with more co-morbidities
Does Anti-Malaria Medication Cure it?
There has been discussion about anti-malarial drugs, Chloroquine and Hydroxychloroquine being used to treat COVID-19. The theory is that although these aren't anti-viral agents they affect the acidity of a part of cells called the Golgi apparatus which the COVID-19 virus hijacks to replicate. By changing the pH of the Golgi apparatus they could slow the virus replication. It is important to point that a lot of evidence for this comes from an in vitro (cells in a petri dish) study, not in human beings
The study which is often being quoted as 'proving' that Hydroxychloroquine works in combination with an antibiotic Azithromycin is Gautret et al. (2020). This study compared treatment with Hydroxychloroquine and Azithromycin, treatment with Hydroxychloroquine alone and standard treatment. This study found that Hydroxychloroquine increased elimination of COVID-19 by day 6 and the effect was improved if Azithromycin was used as well
All studies have their limitations and this one has a few. It is a small study (42 patients) with 26 patients in the treatment arm. Of those treatment patients 6 dropped out and so weren't included in the results. Of these 3 patients went to intensive care, 1 died and 1 dropped out due to nausea from the Azithromycin. These 5 patients could all be considered failures and yet were not included in the results. This made it more likely to find that treatment worked. The study also used nasopharyngeal swabs to detect the virus which we know have a high false negative rate
Basically, more high quality research is needed. Moreover, both Hydroxychloroquine and Azithromycin can cause heart arrhythmia and shouldn't be taken without medical advice anyway. On top of this Hydroxychloroquine is often taken by patients with conditions such as lupus and rheumatoid arthritis who rely on there being a stock
Another drug being investigated is Remdesivir for cases of moderate or severe COVID-19. This drug was developed during the Ebola epidemic on 2014-2016. Both Ebola and COVID-19 use RNA rather than DNA as their genetic material. Remdesivir is designed to interfere with the action of RNA-dependent RNA polymerase, the enzyme RNA viruses use during their replication
Should I Wear a Surgical Mask and Gloves When I’m Outside?
The large respiratory droplets which spread COVID-19 do not typically spread beyond 2 metres and so a surgical mask is only of benefit if you are within 2 metres of someone who is symptomatic.
Using a scarf or homemade mask is of no benefit. Medical gloves do not repel COVID-19 so if you wear them and touch your face they can transmit the virus. If you do wear them you need to either change them regularly or wash them as you would your own hands
How Long is the Lockdown Going to Be?
The UK lockdown is due to be reviewed on April 13th. However, it is very likely that the lockdown will be extended. Wuhan was in lockdown from 23rd January to 27th March. It's estimated that the decision to maintain the lockdown until the end of March and not the beginning prevented 24% infections by the end of the year
References
Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Confirmed 2019 Novel Coronavirus (2019-nCoV) or Patients Under Investigation for 2019-nCoV in Healthcare Settings. February 3, 2020. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/infection-control.html (Accessed on March 11, 2020)
KCDC. Updates on COVID-19 in Korea. March 14, 2020. https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030 (Accessed on March 14, 2020).
Centers for Disease Control and Prevention. Interim Clinical Guidance for Management of Patients with Confirmed 2019 Novel Coronavirus (2019-nCoV) Infection, Updated February 12, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html (Accessed on February 14, 2020
Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Li J, Zhao D, Xu D, Gong Q, Liao J, Yang H, Hou W, Zhang Y Lancet. 2020;395(10226):809. Epub 2020 Feb 12
European Medicines Agency. EMA gives advice on the use of non-steroidal anti-inflammatories for COVID-19 https://www.ema.europa.eu/en/news/ema-gives-advice-use-non-steroidal-anti-inflammatories-covid-19 (Accessed on March 19, 2020).
https://www.entuk.org/sites/default/files/files/Loss%20of%20sense%20of%20smell%20as%20marker%20of%20COVID.pdf
Gautret et al. (2020) Hydroxychloroquine and azithromycin as a treatment of COVID‐19: results of an open‐label non‐randomized clinical trial. International Journal of Antimicrobial Agents – In Press 17 March 2020 DOI:10.1016/j.ijantimicag.2020.105949.
Gilead. Gilead Sciences Statement on the Company’s Ongoing Response to the 2019 Novel Coronavirus (2019-nCoV). https://www.gilead.com/news-and-press/company-statements/gilead-sciences-statement-on-the-company-ongoing-response-to-the-2019-new-coronavirus (Accessed on February 02, 2020).
https://www.gov.uk/government/publications/covid-19-stay-at-home-guidance/stay-at-home-guidance-for-households-with-possible-coronavirus-covid-19-infection
Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response.Grasselli G, Pesenti A, Cecconi M JAMA. 2020
Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, Li S, He J Lancet Oncol. 2020;21(3):335. Epub 2020 Feb 14
Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy Onder G, Rezza G, and Brusafero S JAMA. 2020
Prem, K., Liu, Y., Russell, T., Kucharski, A., Eggo, R., Davies, N., Group, C., Jit, M. and Klepac, P., 2020. The Effect of Control Strategies that Reduce Social Mixing on Outcomes of the COVID-19 Epidemic in Wuhan, China. SSRN Electronic Journal,.
Qiao J Lancet. 2020;395(10226):760. Epub 2020 Feb 12
Association Between Renin-Angiotensin System Blockade Discontinuation and All-Cause Mortality Among Persons With Low Estimated Glomerular Filtration Rate. Qiao Y, Shin JI, Chen TK, Inker LA, Coresh J, Alexander GC, Jackson JW, Chang AR, Grams ME SOJAMA Intern Med. 2020
Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C Lancet Infect Dis. 2020;
Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z JAMA. 2020
A case report of neonatal COVID-19 infection in China. Wang S, Guo L, Chen L, Liu W, Cao Y, Zhang J, Feng L SOClin Infect Dis. 2020
Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA. Published online March 11, 2020. doi:10.1001/jama.2020.3786
World Health Organization. Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (Accessed on February 12, 2020).
World Health Organization. Coronavirus disease (COVID-19) technical guidance: Surveillance and case definitions. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/surveillance-and-case-definitions (Accessed on February 28, 2020).
Updated: WHO Now Doesn't Recommend Avoiding Ibuprofen For COVID-19 Symptoms. Science Alert 2020. https://www.sciencealert.com/who-recommends-to-avoid-taking-ibuprofen-for-covid-19-symptoms (Accessed on March 19, 2020)
World Health Organization. Novel Coronavirus (2019-nCoV) technical guidance: Patient management. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/patient-management (Accessed on February 02, 2020).
https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf
Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention.Wu Z, McGoogan JM JAMA. 2020
Chest CT for Typical 2019-nCoV Pneumonia: Relationship to Negative RT-PCR Testing. Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J Radiology. 2020
In Vitro Antiviral Activity and Projection of Optimized Dosing Design of Hydroxychloroquine for the Treatment of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Yao X, Ye F, Zhang M, Cui C, Huang B, Niu P, Liu X, Zhao L, Dong E, Song C, Zhan S, Lu R, Li H, Tan W, Liu D Clin Infect Dis. 2020;
https://www.youtube.com/user/publichealthengland
Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study.Zhao W, Zhong Z, Xie X, Yu Q, Liu J AJR Am J Roentgenol. 2020;
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B Lancet. 2020
Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, Xia S, Zhou W SOTransl Pediatr. 2020;9(1):51.


![1[1].png](https://images.squarespace-cdn.com/content/v1/592a110b44024329b94b5791/1587119232480-DS2Z6BUUF421QFAHCCKG/1%5B1%5D.png)
![2[1].png](https://images.squarespace-cdn.com/content/v1/592a110b44024329b94b5791/1587119265267-50E2XOQDE54MYCWVIID1/2%5B1%5D.png)
![3[1].png](https://images.squarespace-cdn.com/content/v1/592a110b44024329b94b5791/1587119277339-ZFE3RYOWLBIRZV4MSGOE/3%5B1%5D.png)