You've Got Some Ex-Spleening to Do
A man in his 60s with a background of haemolytic anaemia attends with sudden onset LUQ pain. It's sharp in nature and doesn't radiate. It's severe. He otherwise feels well. There is no history of trauma. He had an ultrasound scan 5 years ago which showed a slightly enlarged spleen. On palpation you think you can feel splenomegaly.
What and where is the spleen?
The spleen is a major haemopoeitic organ with roles in immunity and filtering the blood for cells and bacteria. At any one time about 1/3 of our total platelets will be sequestered in the spleen. Due to this filtration role an enlarged spleen is an important differential in any type of cytopenia.
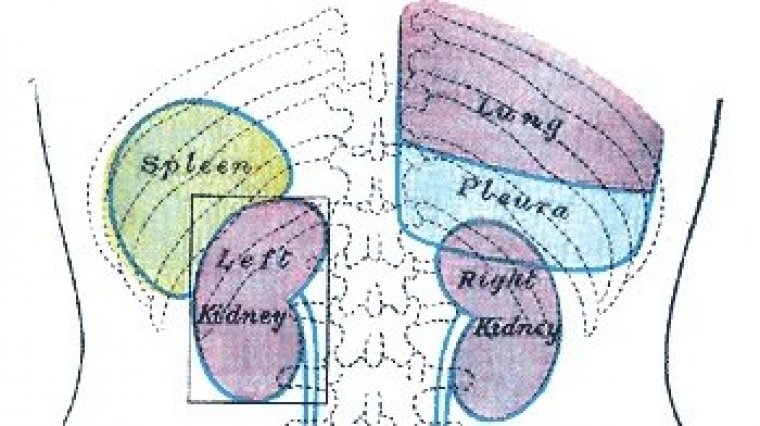
The spleen sits in the posterior left upper quadrant of the peritoneal cavity adjacent to the left 9th-11th ribs, stomach, colon and left kidney; it's hilum is related to the tail of pancreas.
Pictures from Gray's Anatomy.
A normal spleen should not be palpable apart from children, adolescents or very skinny adults. An enlarged spleen is best felt during deep inspiration as this pushes the spleen down against your hands.
Differentials of splenomegaly(1)
● Liver disease – 33 percent (cirrhosis)
● Hematologic malignancy – 27 percent (lymphoma)
● Infection – 23 percent (AIDS, endocarditis)
● Congestion or inflammation – 8 percent (congestive failure)
● Primary splenic disease – 4 percent (splenic vein thrombosis)
● Other or unknown – 5 percent
What could be causing his pain?
Splenic rupture - in 60% of cases of abdominal trauma the spleen is the only intraperitoneal organ damaged. Atraumatic splenic rupture is rare but potentially life threatening(2) with 6 major causes identified in the literature(3):
● Neoplasm (eg, leukemia, lymphoma) – 30 percent
● Infection (eg, infectious mononucleosis, CMV, HIV, endocarditis, malaria) – 27 percent
● Inflammatory disease/non-infectious disorders (eg, acute and chronic pancreatitis) – 20 percent
● Drug and treatment related (eg, anticoagulation, G-CSF, thrombolytic therapy, dialysis) – 9 percent
● Mechanical causes (eg, pregnancy-related, congestive splenomegaly) – 7 percent
● Idiopathic (normal spleen) – 7 percent
Splenic infarct - classical presentation is with acute LUQ pain and tenderness; caused when the splenic artery or one or more of its sub-branches becomes occluded either by an embolus, infective or otherwise. Risk factors include splenomegaly and any pro-thrombotic or pro-embolic state.
Splenic artery aneurysm - the 3rd most common aneurysm in the abdomen after aortic and iliac artery aneurysm.
Splenic abscess - uncommon infection caused by seeding from another site such as endocarditis. Typically presents with persistent fever, LUQ pain with or without splenomegaly.
Learning Points:
- The spleen is higher up than you might think and at risk of injury if the lower left ribs are involved. Always suspect in handlebar injuries
- The spleen must be palpated for properly or you might miss splenomegaly
- Splenomegaly is a major risk factor for splenic pathology; always take a Haematology history and ask about symptoms such as night sweats if you suspect
References:
(1) O'Reilly RA; Splenomegaly in 2,505 patients at a large university medical center from 1913 to 1995. 1963 to 1995: 449 patients; West J Med. 1998;169(2):88.
(2) Carlin F, Walker AB, Pappachan JM ; Spontaneous splenic rupture in an intravenous drug abuser; Am J Med. 2014 Mar;127(3):e7-8. Epub 2013 Oct 29.
(3) Renzulli P, Hostettler A, Schoepfer AM, Gloor B; Systematic review of atraumatic splenic rupture; Candinas D; Br J Surg. 2009;96(10):1114.
Cartoons courtesy of the always excellent Amazing Yeti.