ABCDE of Chest X-Ray - Use the RIPE Approach!
In this podcast Dr. Harry Pick, Respiratory Registrar and Clinical Research Fellow at Nottingham University Hospitals NHS Trust came down to talk us through Chest X-ray Interpretation; a key skill in the Emergency Department!
Harry very kindly gave us a copy of the Powerpoint he uses when he teaches this topic; due to confidentiality reasons these slides don't have X-rays on them but great resources can be found at Radiology Masterclass. Click either side of the pictures to move through them.
Remember the step by step approach:
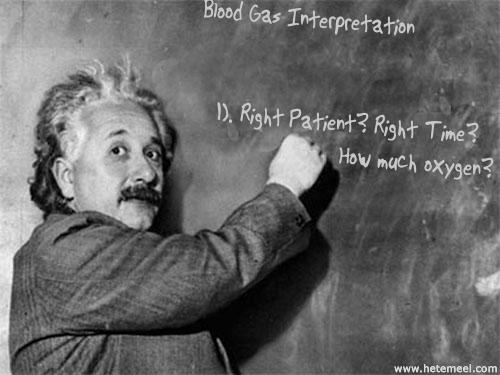
Right patient; day and time? - this is key for all investigations.
Is the film AP (anterior to posterior) or PA (posterior to anterior). This matters for two reasons. Firstly, an AP film tends to be an portable CXR and so tells you that the patient was sick when it was taken, this may be confirmed by the presence of chest leads, O2 tubes and central lines on the film. Secondly AP films exaggerate the size of the heart and so you cannot comment on cardiomegaly. You can on a PA film. In a healthy individual the heart should be no more than 50% of the thoracic width on a PA film. If the scapulae are not projected into the chest assume it is a PA film. It should always say if it is an AP film.
'RIPE' - Rotation (equal space between medial aspects of clavicles to spinous processes), Inspiration (>7 anterior and 9 posterior ribs, Picture (can you see everything you want to see?) and Exposure (can you see vertebral bodies behind the heart).
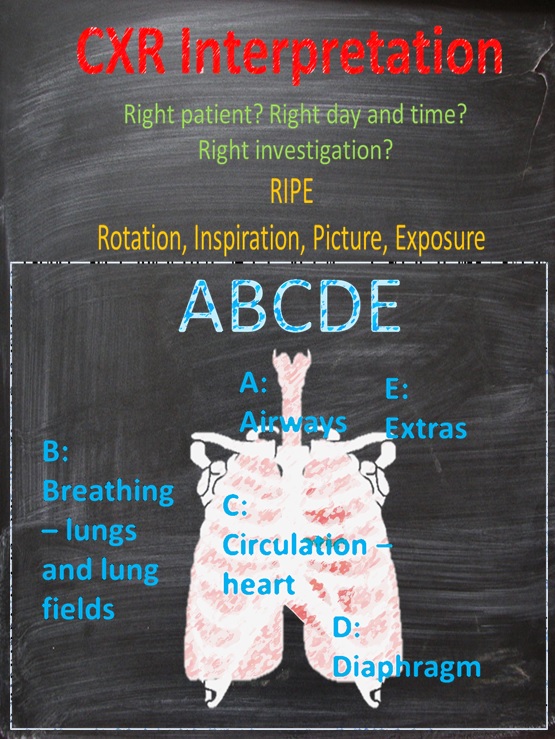
Then remember ABCDE - this varies - the Take Visually below follows Airway, Breathing, Circulation, Diaphragm and Everything else.
Harry's ABCDE covers the same things but in a different order - Apices, Behind the heart, Cardiophrenic and Costophrenic angles, Diaphragms - above and below and Everything else.
Don't forget to compare the chest x-ray with any previous ones (very easy on most programmes) - this is very useful to assess any acute changes. Older x-rays should also have been reported which will help your interpretation!
As you can see there's a subtle variation, make sure you find a method that works for you!
Here is the Take Visually for this podcast.
Geeky Medics have a great page on the subject as well.